A medical device is an item that treats, cures, or prevents certain diseases and health conditions. Doctors and medical professionals use them in hospitals and outpatient facilities, and consumers can buy devices to use at home. Since they are so crucial for good health, the manufacturers must follow strict guidelines.
Medical devices have specific purposes, so the label must adequately share all relevant information. A label should show the consumer how to use the device while also giving information about the manufacturer. This transparency helps consumers understand that medical devices meet professional FDA regulations.
There are certain entities that handle the certifications of medical devices. The requirements can vary depending on who does the labeling. In many cases, it’s the initial manufacturer. But there are re-packagers and kit assemblers involved in the medical field, so their work may impact the labeling process.
Types of Labels Required

The Food and Drug Administration (FDA) helps manufacturers classify medical devices by determining their purpose or searching a database for similar items. From there, you’ll understand what labels you need to put on your device.
As requirements vary depending on the device, checking the regulations before selling products is crucial for compliance. Industries that outsource medical device assembly should verify labels follow FDA regulations before putting their products on the market.
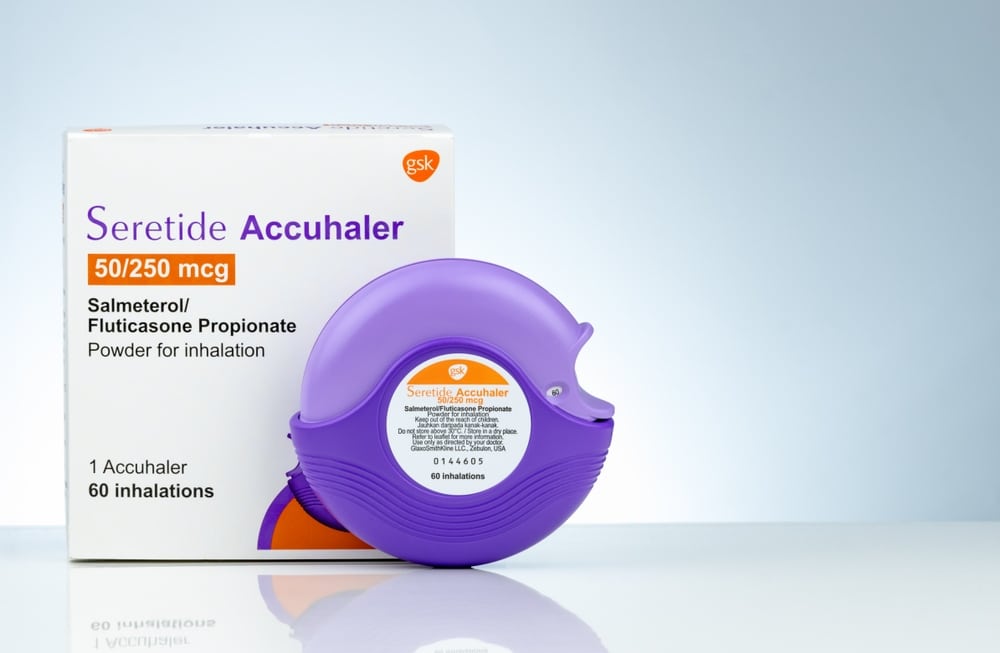
Product Labeling
Product labeling must present all important information to the consumer. FDA regulations require that manufacturers print labels on products that include details like:
- Brand name
- Device identifier
- Details about the production lot
- Expiration date
- Storage and handling
- Unique device identifier (UDI)
The information on the product ensures that consumers can get help even if they lose the external packaging and instructions. There is enough information about the manufacturer and support that they can use the UDI to access the lost information.
Manufacturers connect the UDI to the Global Unique Device Identification Database (GUDID). The FDA oversees this database to help consumers while ensuring that manufacturers stay in compliance with best labeling practices.
Packaging Labeling
Package labeling must include ingredients, usage guidelines, and information about the manufacturer. Nothing can obstruct the label, such as stickers or packaging that isn’t transparent. Customers should have full access to all information before purchasing a product.
The FDA regulations require manufacturers to print information, such as:
- Name and business location
- Purpose of the device
- Instructions for proper usage
The customer can see that data when they pick up the medical device in the store or hospital. They understand if the product will suit their needs and have an idea of how to use it. Detailed instructions inside can provide more information or help with any questions, but the packaging gives a broad overview.
Manufacturers also include information from the device on the external packaging. This process helps link the physical device with the box by UDI. If there’s an issue with the device, label, or packaging, it’s easier to track everything through the GUDID.
Information Included on Labels
Medical device manufacturers include crucial information on the label to help identify each device, protect consumers from counterfeit devices, and simplify the recall process if necessary.
When people shop for medical devices, they know to look for certain information and symbols to purchase a legitimate product instead of making false promises. The FDA guidelines prevent medical device manufacturers from making broad claims that give consumers false expectations, making them focus on the facts about the device.
Each medical device package needs to have clear labels with the following information:
- Product name
- Manufacturer name and location
- Customer support number or website
- Model, catalog, or part number
- Serial number, if applicable
- CE marking, if applicable
- Unique Device Identifier (UDI)
The product name helps from the packaging process until the consumer purchases the medical device. It helps ensure employees put the correct item in the matching box, so the customer gets the product they need. The name also helps consumers find the product on store shelves without confusion regarding what they’re buying.
The manufacturer’s name and location provide transparency for the consumer. They know what company made the device and where they have headquarters. If a consumer isn’t buying the device based on a doctor’s recommendation, this information helps them research the company themselves.
A customer support phone number or website also empowers the consumer. They can contact the manufacturer to ensure they’re choosing the right product. If they lose the internal instructions, they have a way to contact the company for more information.
The model, catalog, or part number helps during the manufacturing process to ensure workers put the right elements together in the package. It also helps the manufacturer keep track of the devices made, shipped, and sold. The FDA keeps this information on file to ensure the company is compliant.
The serial number also helps the manufacturer and FDA keep track of medical devices. The previous information sometimes eliminates the need for a serial number.
The CE marking refers to a symbol used in Europe. If a manufacturer plans to sell their medical devices in European countries, they need to apply for and earn the CE marking. It shows consumers that the product aligns with Europe’s health and safety standards.
The UDI looks like a string of numbers, but manufacturers and the FDA read it like code. The digits give information about the device model and its production. The numbers help manufacturers pull data on the production lot, batch number, and expiration date from their records.
The UDI system simplifies the medical device manufacturing process. It allows for accurate record-keeping regarding device production, usage, and defects. Since the UDI links to a production lot, manufacturers can quickly issue recalls to all customers with an affected device.
Medical professionals using medical devices always have relevant information at their fingertips. They can use the UDI to access data about the device and proper usage to ensure they keep their patients safe.
Additional Labeling Requirements Depending on Medical Device Type
The previously mentioned label requirements might seem like a lot of information to include on a package and device, but that’s not everything a manufacturer needs to consider. There are additional labeling requirements depending on the type of medical device.
Class I Devices
Class I medical devices have low risk. They don’t have a significant impact on a patient’s health, so manufacturers don’t need to follow strict guidelines with these products. The devices don’t touch a patient’s cardiovascular system, central nervous system, or internal organs.
The FDA estimates that 47% of medical devices are Class I. Some examples include:
- Bandages
- Latex gloves
- Stethoscopes
- Surgical masks
- Tongue depressors
These devices won’t save or sustain a patient’s life, but they’re necessary for medical procedures. There’s less risk involved with using these devices, so they have more relaxed FDA requirements regarding labeling.
Class IIa and IIb Devices
Class II medical devices have an intermediate risk. Since there’s variation in the intermediate levels, the FDA breaks Class II into sections. Class IIa contains medical devices with low to medium risks to the patient’s health. Class IIb medical devices have medium to high risk.
Class IIa devices go inside a patient’s body but aren’t a permanent addition. Examples include:
- Blood transfusion tubes
- Catheters
- Hearing aids
Class IIb devices are invasive. Medical professionals can insert them during surgery because they’re more likely to improve a patient’s health than create a health risk for them. Examples include:
- Intensive care monitoring equipment
- Intraocular lenses
- Ventilators
Since Class II devices put consumers at some risk, they must follow special labeling guidelines from the FDA. Manufacturers also conduct regular testing to ensure they meet performance standards.
Class III Devices
Class III devices pose the most risk for consumers. Because of the risk, the FDA labeling guidelines are strict. These products follow all regulations for Classes I and II, plus they must have pre-market approval from the FDA. The organization requires a scientific review of the device to ensure it can support or sustain the patient’s life.
Examples of Class III medical devices include:
- Breast implants
- Defibrillators
- Pacemakers
In Vitro Diagnostic Medical Devices
In vitro diagnostic medical devices have their own category from the FDA. It includes any instruments, systems, and tests that determine the state of health by taking biological samples from the patient. Examples of these devices include:
- Blood glucose tests
- Diabetic tests
- Pregnancy tests
Manufacturers must label these products with the same information as the other classes of medical devices. They require the addition of a risk-based classification:
- Class A: low individual and public health risks
- Class B: moderate individual and low public health risks
- Class C: high individual and moderate public health risks
- Class D: high individual and public health risks
Labeling must also provide traceability with the UDI so the manufacturer gives the public complete transparency regarding production and usage. The FDA also requires heightened post-market testing on the devices to ensure there are no usage issues.
Best Practices for Maintaining Medical Device Labeling Compliance
Medical device labeling compliance includes crucial features such as having a risk management plan and maintaining a quality management system. If your company routinely reviews compliance standards, you’ll always meet the proper FDA regulations.
There are industry-wide compliance standards, like ISO 13485, which outline the guidelines for medical device manufacturers. The standard states that manufacturers need to meet customer and industry regulations involving the design, production, storage, and distribution of medical devices.
Risk Management Plan
A risk management plan for medical devices shows the proper use of the medical device while also exploring potential problems that arise with proper or improper use. The manufacturer needs to stay aware of issues that might happen when the public uses the medical device.
Ideally, the manufacturers design a product so it won’t fail. They test every potential outcome with a prototype to see what might happen with regular use. If a manufacturer sees problems with the device, they need to go back to the drawing board and reevaluate the design to make it safer.
At a certain point, the manufacturer can’t eliminate all chances of risk. At that point, they need to add a section to the risk management plan that shows the low associated risk and get approval for the device as-is.
Quality Management System
The quality management system outlines the process involved with designing, manufacturing, storing, and supplying medical devices to professionals and the general public. It also oversees complaints, clinical data, and product labeling. Maintaining your quality management system means you’re keeping all aspects of the business in order.
Get Help With Medical Device Labeling
There are many medical devices on the market. They all need clear labeling so manufacturers can track production, maintain federal compliance, and inform consumers about the product.
Since there are many different classes of devices, you should carefully follow the regulations for your specific product. This approach ensures you comply with FDA regulations and promote safety and quality for your business. Medical device businesses can help with labeling compliance. Contact MDI today to learn how we can help.